study was carried out to demonstrate how a biotribometer can be used to understand the tribological interactions between silicone breast implants and models of tissues found within the breast pocket.
The study built a general understanding of how breast implant surface texturing may induce tissue damage
Fluorescence imaging showed that for smoother breast implants, normal and friction surfaces were distributed over larger surface areas, leading to lower frictional shear stresses.
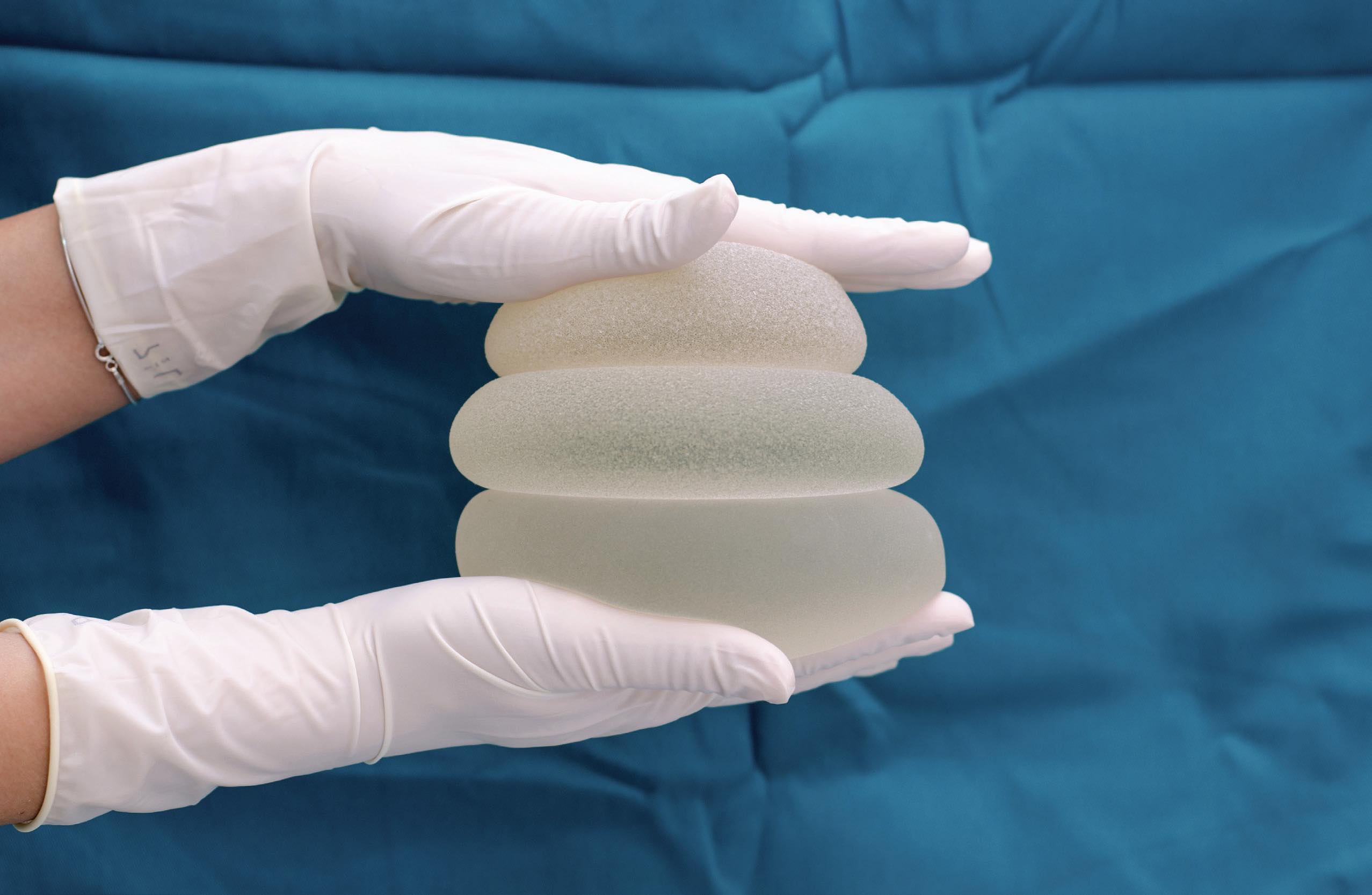
Roughly one in eight cancer diagnoses worldwide is breast cancer. In 2020, there were over two million new cases of breast cancer globally and nearly 700,000 deaths from this disease. Approximately 100,000 breast reconstructions are performed each year, with 82% being implant-based. While silicone breast implants have been used since the 1960s, advancements in breast implant materials and technology have lagged. The leading material used in breast implants is predominantly silicone elastomers, which also can be found in shunts, biosensors and other medical prostheses. However, certain types of silicone breast implants have been linked to adverse reactions ranging from inflammation to lymphoma, a cancer of the immune system. To date, the role of friction in breast implant complications remains largely underexplored.
STLE member Jonah Rosas is a fourthyear graduate student researcher in the Biomolecular Science and Engineering Department at the University of California, Santa Barbara, and has been conducting research in the Interfacial Engineering Laboratory led by STLE member professor Angela Pitenis. Rosas recently led efforts to understand the fundamental mechanisms of friction-induced complications associated with breast implant materials. He says, “In general, biological tissues have not evolved to accommodate the frictional shear stresses reacting across the implant-tissue tribological interfaces. This is particularly concerning for breast implants with intentionally roughened surface textures.”
Rosas continues, “Designers of breast implants originally hypothesized that aggressively textured surface profiles would help keep breast implants from moving out of place, in a manner reminiscent of Velcro. However, the reality is that even textured breast implants move around in the body, which can lead to scarring within the breast pocket and usher in more serious complications.”
The foreign body response (FBR), which Rosas explains is the body’s initial response to a breast implant and a part of the wound healing response, generates immediate inflammation at the site of the newly im- HIGHLIGHTS An
in vitro study was carried out to demonstrate how a biotribometer can be used to understand the tribological interactions between silicone breast implants and models of tissues found within the breast pocket. The study built a general understanding of how breast implant surface texturing may induce tissue damage
in vivo. Fluorescence imaging showed that for smoother breast implants, normal and friction surfaces were distributed over larger surface areas, leading to lower frictional shear stresses. planted device and then promotes scarring over time. He says, “When a foreign object is placed in the body, the body responds by creating a capsule around it, which is essentially a three-dimensional network of proteins, primarily composed of collagens. This capsule literally walls off the implant from the rest of the body. In the case of extremely rough surface profiles (average surface roughness, Ra >50 microns), the initially formed capsule may be insufficient to completely wall off the implant, which may lead to excessive scarring but could also lead to the failure of the implant.”
A better understanding of the tribological interactions between a breast implant and the surrounding tissues is needed to gain a better understanding of what type of medical devices will minimize patient complications. Rosas, Pitenis and their colleagues hypothesized that increasing implant surface roughness would lead to an increase in frictional shear stresses and soft tissue damage and designed an instrument, an
in situ biotribometer, to evaluate the extent to which this may occur
in vitro.
In vitro studies were conducted using a custom linear reciprocating biotribometer mounted to the condenser turret of an inverted laser scanning confocal microscope. Sections of silicone breast implant shells were placed on hydrogel probes fastened to a cantilever assembly.
Rosas says, “Our objective was to better understand the tribological interactions between commercially available silicone breast implants and models of tissues found within the breast pocket, including collagen-coated polyacrylamide hydrogels and healthy breast epithelial cells. Our
in vitro approach enabled us to build a general understanding as to how breast implant surface texturing may induce tissue damage
in vivo.”
Each surface was subject to 1,000 mm of sliding, a distance representative of implant motions within the first three months after medical device implantation into the body. From these studies, Rosas and colleagues were able to determine the coefficients of friction (the difference between the forward and reverse friction forces divided by the average normal force) for implant surfaces tested against both collagen and cell surfaces.
Rosas says, “As part of this study, we were able to continually image each sample in real time to gain a better understanding of the frictional stresses and wear during dynamic sliding. This was particularly effective in determining the apparent contact area between each implant and its respective countersurface during testing. By leveraging high resolution fluorescence imaging, we could visualize damage to our
in vitro models of tissue over time.”
The researchers used fluorescence imaging to find the real area of contact between breast implant probes and each countersurface. Rosas says, “For smoother implants, normal and friction force stresses were distributed over larger surface areas, leading to lower contact pressures and lower frictional shear stresses.”
Further studies are needed to better understand how cell layers and tissues at the sliding interface adapt to frictional shear events. Rosas says, “We hope that an appreciation of biotribology can help inform design considerations for other soft implantable materials such as shunts, catheters and gastric bands to reduce patient complications and increase quality of life.”
Additional information on this work can be found in a recent article
1 or by contacting Rosas at
jonahrosas@ucsb.edu and Pitenis at
apitenis@ucsb.edu.
REFERENCE
1.
Rosas, J., Atkins, D., Chau, A., Chen, Y., Bae, R., Cavanaugh, M., Lima, R., Brodeos, A., Bryant, M. and Pitenis, A. (2022),
“In vitro models of soft tissue damage by implant-associated frictional shear stresses,”
Proceedings of the Institution of Mechanical Engineers, Part J: Journal of Engineering Tribology, https://doi.org/10.1177/13506501221132897.